
-
In this Issue:
- Governor's Welcome
- Chapter News
- ACP National Award: Fred J. Schiffman, MD, MACP
- Doctors Dilemma Competition
- Annual Meeting
- Council Meeting
- Mentorship Zone
- From National ACP

Kwame O. Dapaah-Afriyie, MBchB, FACP, ACP Governor
Governor's Welcome
I hope you all had an enjoyable Thanksgiving holiday with family and friends.
All too soon this year is coming to an end, and we are at the dawn of a new beginning. The varying emotions about our country’s political terrain and other ongoing worldwide events extend to personal and professional lives. The change in the US political terrain for some means a renewed sense of optimism but for others raises serious concerns about the potential erosion of gains made over centuries, decades, years and in some cases months.
Our patients who are experiencing similar varying emotions will be better served by a renewed emphasis on emotional intelligence (EQ) in our interactions with them. Emotional intelligence is not only an admirable attribute, but rather an asset for patient care optimization.
Clinical decision-making is more than a rational and cognitive process. It involves an emotional overlay which we need to be aware of and nurture positively to achieve better quality of care. The resultant enhanced empathy and ability to respond to stressful scenarios have been noted to improve teamwork and enhance career satisfaction.
We will serve ourselves, patients and professional community much better as we work on boosting our EQ in addition to staying abreast with new medical information.
A quick refresher on some aspects of EQ:
The major components of emotional intelligence are:
- Self-awareness - awareness of our emotions is not self-serving. It results in self-attention, care and management which are essential for effective service in our various roles.
- Self-regulation – awareness of the need to control the space between a trigger/stimulus and our responses helps in expressing better choices and enhances our adaptability and calmness under emotionally stressful circumstances.
- Empathy – this helps us understand and respond to needs of others appropriately.
- Social skills – The ability to accurately perceive emotions in other people; the thoughts and feelings driving their behavior enables us to successfully manage relationships and/or conflict to attain desired goals.
The increasing need for emotional intelligence cannot be overemphasized. Our patients, professional well-being and the pursuit of the ideals of humanistic medicine require proficiency in emotional intelligence.
Enjoy the upcoming holiday season!
Chapter News
Committee Highlights: Early Career Physicians
By Sarah Freeman, MD, FACP
Sarah Freeman and her leadership team have worked collaboratively with leadership of the RI Chapter of Society of Hospital Medicine in organizing joint educational programs.
The Committee will be having a Webinar about financial planning in the next few weeks.
Community Initiative: In Spring of 2025, members of this committee in partnership with OASIS RI international (NGO) will start an initiative to provide educational support for its after-school Youth program. The goals include encouraging interest in life sciences and providing information about healthy lifestyles.
ACP National Award: Fred J. Schiffman, MD, MACP
Dr. Fred Schiffman is the recipient of the 2025 Nicholas E. Davies Memorial Scholar Award for Scholarly Activities in the Humanities and History of Medicine.
Fred J. Schiffman, serves as Vice Chairman of the Department of Medicine at the Miriam Hospital. In 2010, Fred was named the inaugural Sigal Family Professor of Humanistic Medicine. Most importantly in his work as an educator and mentor, Dr. Schiffman has served as an Associate Residency Director for Internal Medicine at Brown University for over 30 years, allowing him to make significant contributions to the professional and personal growth of thousands of students, residents and fellows. Dr. Schiffman served as the Governor of the Rhode Island Chapter of the ACP from 2023-2027 and was awarded ACP Mastership in 2015.
Doctor's Dilemma Competition
Our Chapter’s annual Doctor’s dilemma competition was held on November 19Th. The winning team of residents from Landmark Medical Center (Hossam Mustafa, MD, Kanishka Uttam Chandani, MD, Omar Alkasarbrah, MD) will represent our chapter at the National competition which will be held at the April 2025 ACP meeting in New Orleans.
For the few of us who may not be aware of this new residency, it was started in July of 2021 and is sponsored by New York Medical College. There are a total of 36 medical residents in the program. Glenn G. Fort. MD., MPH., FACP., FIDSA is the Program Director.
Special thank you to Dr. Alisha Crowley, Dr. Matt Lynch, and Dr. Lynn Bowlby (our judges) who worked to make this a successful and enjoyable evening.

Hossam Mustafa, MD, Kanishka Uttam Chandani, MD , Omar Alkasabrah, MD

Annual Meeting
Our 2025 Chapter meeting will be held at Kent County Hospital’s Doctor’s auditorium on 03/12/2025.
In addition to the plaques, we are now including cash prizes for the top 3 winners of the podium presentations. Let us encourage our residents to be part of this academic endeavor.
Information soliciting nominations for the 2025-chapter awards will be sent out in Jan 2025.
Council Meeting
The next Governor’s Council meeting which will be a virtual meeting will be held on 12/11/2024.
Mentorship Zone
What are we learning? Who are we learning from? Who are we transferring insights to?
Iron sharpens iron, so one person sharpens another.
The one who waters will also be watered.

In this newsletter, we get to learn from one of our former Governors Kelly McGarry. MD. MACP, and John Miskovsky MD who is the Internal Medicine Program Director at Roger Williams Medical Center. Two experienced colleagues whose insightful perspectives will be beneficial to all of us especially our medical students, residents, and Early Career Physicians.
Kelly McGarry, MD, MACP
I grew up being the first in my family to attend college; there were no role models in medicine or people who could provide support as to what a career in medicine would look like for me. Despite the challenges, it was in middle school that medicine was what I saw myself doing. In choosing medicine, I was following a passion – a dream that I could help support and guide patients as they navigated difficult illnesses through our difficult to navigate health care system. (I like that intentional redundancy) I had some personal experiences in my family where I saw the fear, the uncertainty, and the stress that can result from one’s illness and the system. The doctor that I envisioned could help the most was an internist specializing in primary care. When I got to medical school, I actually did not even know what an “attending” was, but still my north star pointed me to general internal medicine, and I stayed true to that. As I navigated medical school, I found many areas interesting, but never veered from the role that I saw would help me guide, support, and connect with patients the most, that of primary care. I have taken on many roles since medical school in my career, but I have maintained a focus and a commitment to my role as a primary care physician with women’s health expertise and see this as what guides me and centers me in all my other work.
In thinking about factors that have helped me in my profession, I have several I would like to share.
First, mentors and colleagues have been a great source of support as I have navigated my career. Doing this work in isolation, not reaching out to get advice or seek guidance, especially on tough days, is a real missed opportunity as we go through our days. What we do requires serious emotional and mental energy – we are always thinking. Sharing our thoughts and our struggles with friends, colleagues, and mentors is paramount to keeping us doing this important work. I have found the guidance from my mentors and colleagues boundlessly helpful.
The second factor that has helped me along the way is always remembering to keep the patient at the center. They are the “why”. It is easy to let the systems issues distract us or bring us down (there are so many). If we remember that patients seek our help and guidance because they are frightened or just not feeling well, understand that we are their trusted go-to, and recognize that we have so much to offer, we will always find that original joy and meaning which led us to this profession in the first place. I try to remember this every day and multiple times per day on the most challenging days – it’s my mantra.
The third factor I would like to share that has helped me is my philosophy of trying to never take myself too seriously (not always easy, but I try) – in having this philosophy, I think it can help us not be afraid to laugh at ourselves, not be afraid to make and learn from our mistakes, and be open to new thoughts and new experiences, and not be afraid to say we are sorry. Life is too short. It is critical to our own well-being to keep our minds open to experience the grace and privilege along the way of providing care to patients.
There are numerous challenges that threaten what gives us meaning, at the top of which for most is caring for our patients (I won’t use this space to elaborate on the myriad of challenges; we all experience them, and many are suffering because of them). For some of us, there may be additional roles we have that add meaning to our work, whether in administration, advocacy, teaching, or research. We see these challenges every day in our systems that need to function better to help support our ability to reach our “ikigai” (the Japanese concept meaning discovering our purpose through exploring the intersection of what you love, what you are good at, what the world needs, and what you can get paid for). What keeps me motivated despite the many challenges facing our health care system nationally and locally is recognizing that each of us can work to make a difference in the things that need improvement and viewing the many challenges as opportunities. Whether you have been in practice one year or more than thirty years, there are ways to make a difference in areas that are important to you. I would encourage you to think about what drives you, what gives you meaning, what you think needs changing, and talk to those around you to see how you can get involved to make a difference. You may have a great idea that just needs to be heard…share it and see what happens. In my own experience, that practice has made all the difference, and I know it can do likewise for you.
John Miskovsky, MD
I have had the privilege of being part of the medical community in Rhode Island for over 25 years, beginning as a student at Brown Medical School from 1992 to 1996. It was during this time that I developed my initial passion for internal medicine. I was captivated by Charles Carpenter, then chief of medicine at The Miriam Hospital, as he would skillfully dissect each case, when we as third-year medical students, presented to him during our core clerkship sessions. His ability to arrive at a correct diagnosis through detailed questioning and examination was awe-inspiring, and I knew then that internal medicine was the career path I wanted to pursue.
As a fourth-year medicine sub-intern, I recall attending an internal medicine morning report session at Roger Williams Medical Center, where I was struck by the depth of knowledge displayed by the residents about their patients. Following the advice of my mentor, Stephen Zinner, then-chair of medicine at Roger Williams (and at Brown University), who told me there was no better person to learn from than Robert Moellering, the program director at Deaconess Hospital in Boston, I completed my residency training at Beth Israel-Deaconess Medical Center. I returned to Rhode Island to serve as chief medical resident at Memorial Hospital of Rhode Island and I have practiced internal medicine in Rhode Island ever since.
Over the past two decades, I have had the privilege of caring for thousands of patients, both as a hospitalist and a primary care physician in general internal medicine. I have developed relationships with multiple generations of families who have entrusted me with their care. Throughout this time, I have shared in life-altering moments, delivered difficult news, and, above all, felt deeply privileged to hold such significant responsibility.
As internists, people place their lives in our hands, and we must use our knowledge and experience to arrive at the correct diagnoses and devise optimal treatment plans. Even after more than 20 years in practice, I still encounter novel problems and presentations, making my job one of the most challenging and rewarding professions I could imagine.
Along the way, I’ve been fortunate to have many mentors, in addition to those I have mentioned, and I’ve had the honor of working alongside some of the most respected physicians in the state. I hope to pass on the knowledge and experience I’ve gained to the next generation of doctors.
Over the years, I’ve mentored countless students and residents, and I’ve served in several roles in graduate medical education, both at Memorial Hospital of Rhode Island and at Roger Williams Medical Center, where for the past four years I have been the internal medicine residency director. This role has brought me immense personal and professional fulfillment.
Trainees consistently inspire and challenge their mentors, ensuring that we stay sharp, practice to the highest standards, and remain up to date with the latest guidelines. They push us to strive for excellence, refining our skills as clinicians, educators, and mentors. Contributing to the well-being of my patients, as well as countless others through the development of my trainees, is one of the greatest rewards of my career.
Certainly, the last decade has brought its share of challenges and stresses in the practice of medicine, but I truly believe that being an internist is one of the most intellectually stimulating and personally rewarding professions. I cannot imagine doing anything else with my life.
From National ACP
ACP Board of Regents’ actions on key Fall Board of Governors’ meeting resolutions:
Adopted as a Reaffirmation:
2-F24. Advocating for Greater Transparency of Private Equity Acquisitions in Healthcare
3-F24. Providing Physicians with Information on Part B and Part D Medicare Policy
4-F24. Addressing the Negative Impact of Electronic Health Record (EHR) Message Burden on Patients and Physicians
7-F24. Declaring Access to Equitable, Affordable Healthcare is a Human Right
ACP MEMBERSHIP UPDATE: As noted in messages sent from national office a last month, starting February 2025, new post-training ACP members (excluding students, resident/fellow, or transitional medical graduate members) will have their dues renewal dates aligned with their ACP join date rather than ACP’s fiscal year. This change simplifies and streamlines the dues process, eliminating dues pro-ration, and with the aim to increase member retention.
Click here for more information about the new dues structure and auto-renewal savings.
ACP Strategic Priorities (2024-2027)
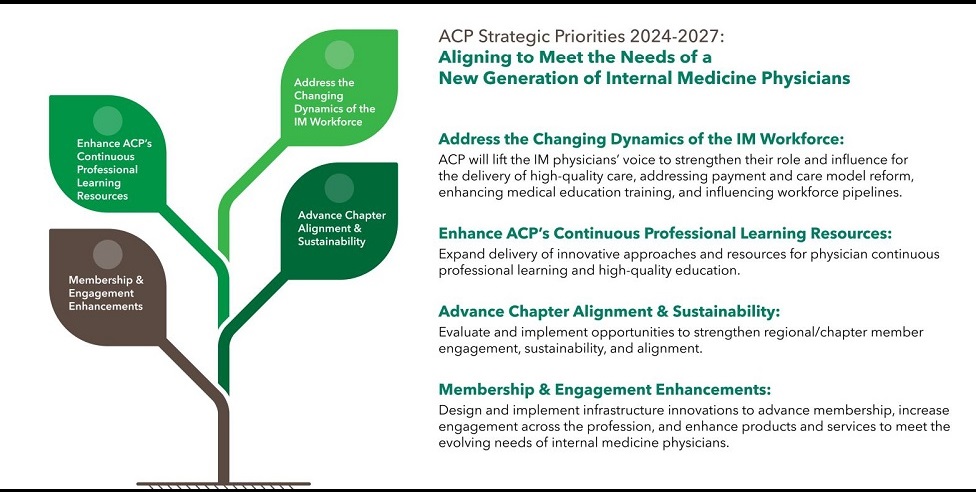
ACP has outlined and initiated steps to align itself and be better positioned to meet the needs of a new generation of Internal Medicine Physicians. The steps will be under the following categories.
A. Address the changing dynamics of IM workforce.
B. Enhance ACPs continuous professional learning resources
C. Membership and engagement enhancements
D. Advance chapter alignment and sustainability

